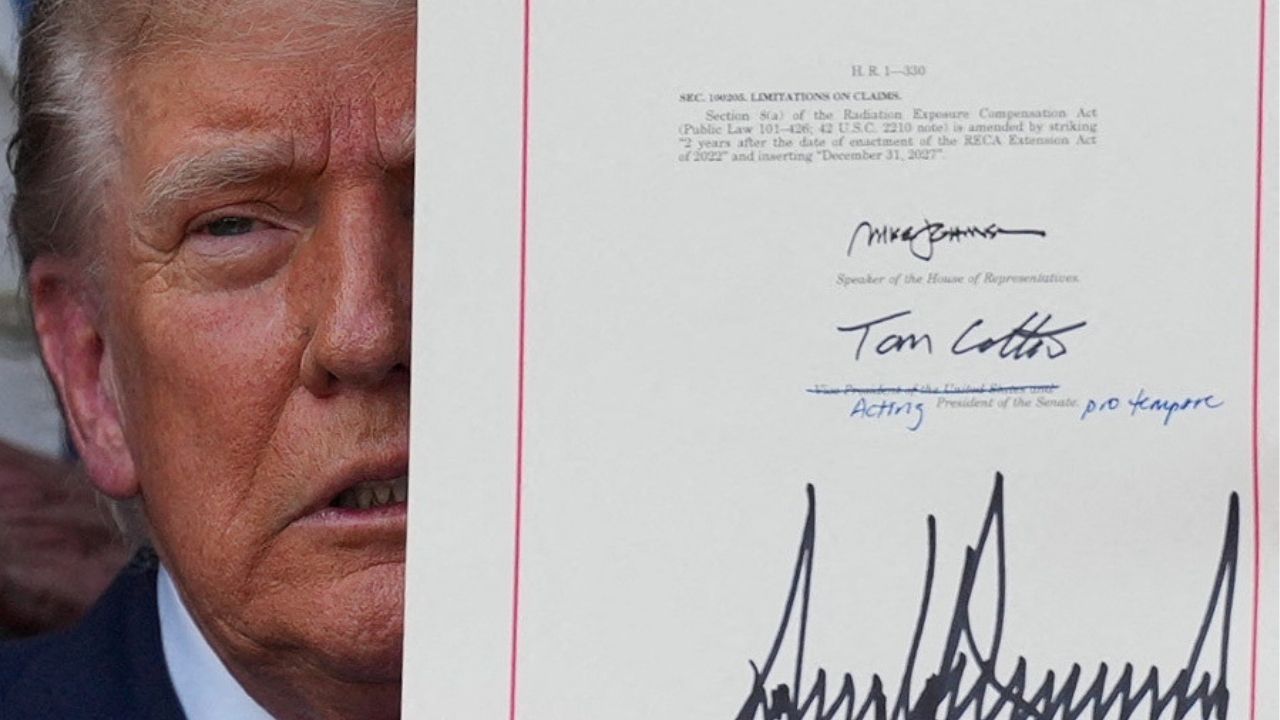
President Donald Trump presents the sweeping spending and tax legislation, known as the "One Big Beautiful Bill Act," after he signed it, at the White House in Washington, D.C., U.S., July 4, 2025. (Reuters File)

- Trump’s Medicaid bill pressures insurers with higher administrative costs and work requirement rules, prompting them to scale back coverage.
- Experts predict millions could lose Medicaid coverage as states struggle with new verification mandates under Trump's healthcare spending bill.
- Insurers may exit markets, boost perks, and raise administrative spending to retain healthier Medicaid members amid looming federal policy shifts.
Share
|
Getting your Trinity Audio player ready...
|
NEW YORK – President Donald Trump’s spending bill is set to raise administrative costs and make managing costs more difficult for insurers like UnitedHealthcare and CVS Health’s Aetna that operate Medicaid health plans, experts say.
As a result, those insurers will likely pull back their Medicaid coverage and invest more in existing markets to retain their healthier members, experts said.
States contract with insurers, including UnitedHealth Group’s UnitedHealthcare, CVS Health’s Aetna, Centene and Molina , to operate Medicaid plans that are jointly funded by state and federal governments.
Almost all of Molina’s and nearly half of Centene’s insurance business is composed of Medicaid members. That portion is smaller for Aetna and UnitedHealthcare which operate large commercial businesses.
Seven industry experts say the bill’s funding cuts and its stipulation requiring states to verify patients’ work status deliver a blow to insurers.
The provision in Trump’s One Big Beautiful Bill Act requires low-income adults, in states that have expanded Medicaid coverage under the Affordable Care Act, to prove every six months that they meet work requirements in order to maintain coverage.
State Medicaid departments, grappling with scant operational teams, will have a difficult time carrying out verification protocols, five industry experts said.
“The expectation is that states are going to have to be ready by 2026 or 2027, and that’s a fast turnaround window,” said Nikita Singareddy, CEO of healthcare platform Fortuna Health.
A spokesperson for Centene said it would work with federal and state partners to help patients navigate change.
A spokesperson for CVS Health declined to comment. UnitedHealth Group and Molina did not immediately respond to a Reuters request for comment.
For insurers, the disruptions could result in more sick people enrolled in the Medicaid plans they operate on behalf of the government because those who are more ill are likely to complete the verification process because they have an immediate need for healthcare, industry experts and an investor said.
The Congressional Budget Office estimated Medicaid policy changes in the bill could leave 7.8 million people uninsured by 2034. Mass disenrollment could begin in 2027 on a rolling basis, according to an expert at a state policy organization.
The White House did not immediately respond to a request for comment.
States may choose to pay companies operating health plans at lower rates due to funding cuts, said Eric Levine, a principal consultant at Avalere Health.
Following the COVID-19 pandemic, insurers have said the rates they are paid by states have not caught up to actual cost of care.
Disenrollment of healthy people may exacerbate this misalignment, leading to inaccurate rates paid to plans and squeezed profit margins, according to a spokesperson for a national insurance trade organization and an investor.
‘Another Period of Retrenchment’.
If insurers find the fallout from these changes daunting, they are likely to exit certain markets or pull back on bidding or competing for footprints in new areas.
“Insurers will continue to be more cautious about not just entering any new states, but retrenching just in the states where they have the highest market share, most scale and more profitable business,” said Jeff Jonas, a portfolio manager at Gabelli Funds, which owns shares of UnitedHealth Group.
In an effort to keep healthier patients that drive profits enrolled, insurers may employ plan design changes ahead of the bill’s finalization, adding perks that can make enrollment more appealing.
This could help insurers retain and attract healthy members, according to Matt Salo, CEO of Salo Health Strategies and founding director of the National Association of Medicaid Directors and two other policy experts.
Hosting volunteer events and job or educational search services are strategies insurers may use to engage members and reduce losses, said Levine.
Health plans are also expected to boost transportation benefits and other social-need benefits for low-income Americans. Jonas and a spokesperson for a national health insurer say this programming will boost administrative costs in the short-term.
—
(Reporting by Amina Niasse; Editing by Michael Erman and Anna Driver)