Share
I, like many Americans, miss the pre-pandemic world of hugging family and friends, going to work and having dinner at a restaurant. A protective vaccine for SARS-Cov2 is likely to be the most effective public health tool to get back to that world.

Opinion
Marcos E. García-Ojeda
The Conversation
Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, cautiously estimates that a vaccine could be available in 12 to 18 months.
I am a professor of microbiology and immunology and study how the immune system develops. I think Dr. Fauci’s estimate is an optimistic one, but possible.
Traditional vaccine development is a long and complicated process. Only about 6% of vaccine candidates are eventually approved for public use, and the process takes 10.7 years, on average.
But these are not traditional times. Researchers around the world are innovating the process of vaccine development in real time to develop a vaccine as fast as possible. So how close are we to a vaccine?

A Step-By-Step Process
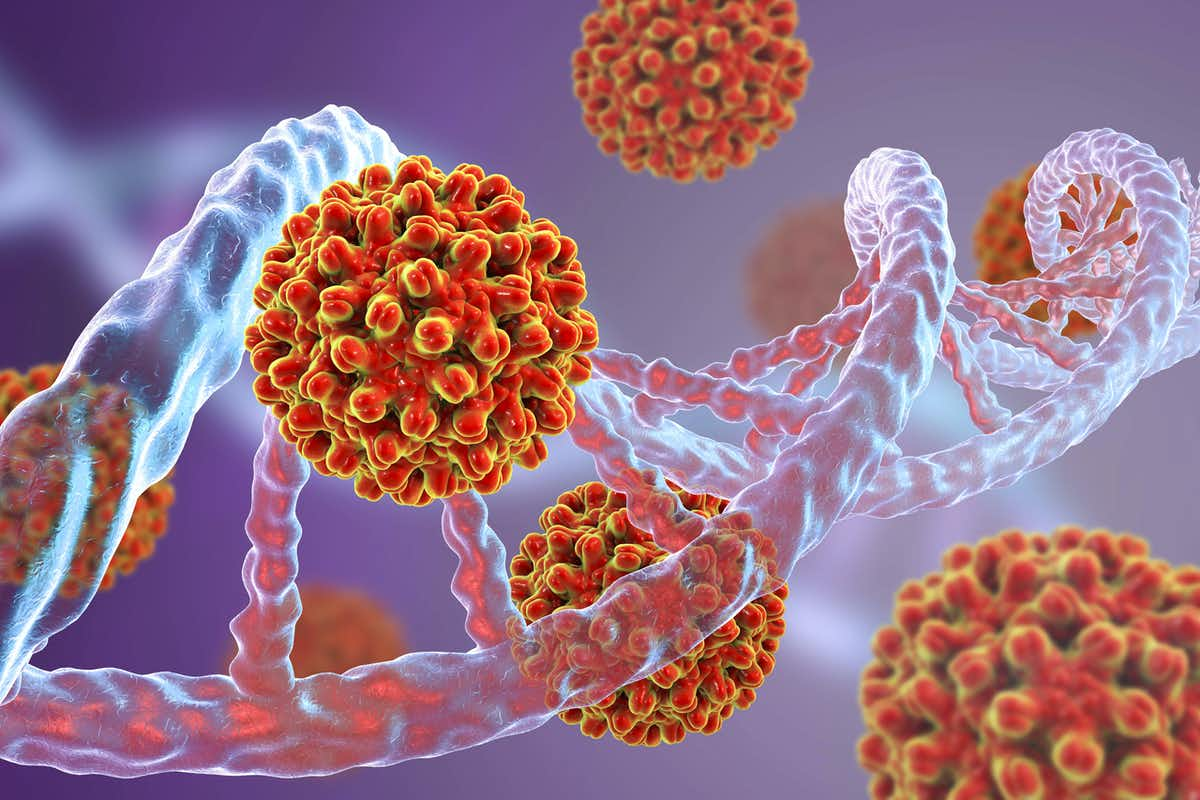
Vaccines prevent disease by boosting a person’s natural immune response against a microbe that they have not encountered before. There are a number of different types of vaccines in development for SARS-CoV-2 and they fall into three broad categories: traditional killed-virus vaccines, protein-based vaccines and gene-based vaccines. No matter the type, every single vaccine candidate must go through the same vetting process before it can be put into use.
Once researchers have developed a potential candidate, they begin the first step of testing in laboratories, called preclinical studies. Scientists use laboratory animals to examine if the candidate vaccine induces an immune response to the virus and to check whether the vaccine causes any obvious medical problems.
Once a vaccine is proven safe in animals, researchers begin human testing. This is where the federal Food and Drug Administration begins to regulate the process.
Phase 1 studies test for safety and proof-of-concept. Researchers give a small number of human volunteers the vaccine. Then they look for medical problems and see if it induces some sort of immune response.
In Phase 2 studies, researchers give the vaccine to hundreds of volunteers to determine the optimal vaccine composition, dose and vaccination schedule.
The final step before a vaccine is approved by the FDA for broad use is a Phase 3 trial. These involve thousands of volunteers and provide data on how good the vaccine is at preventing infection. These large trials will also uncover rarer side effects or health issues that may not show up in the smaller trials.

If in any of these phases a vaccine candidate appears to be ineffective or cause harm to people, the researchers must start over with a new candidate.
After a vaccine candidate successfully completes these clinical trials, a medical regulatory panel in the FDA looks at the evidence, and if the vaccine is effective and safe, approves it for general use. Experts estimate that the whole process costs between US$1 billion and $5 billion.
But approval is not the only hurdle. As has been demonstrated by the severe lack of coronavirus testing, easy and fast production of a test or vaccine is as critical as having one that works.
Both clinical efficacy and ease of production must be considered when asking how long until a vaccine is ready.
Current Promising Candidates
As of April 30, 2020, there were eight vaccine candidates currently in Phase 1 (or joint Phase 1/Phase 2) clinical trials and 94 vaccines candidates in preclinical studies.
Three of the eight are traditional vaccines that use inactivated or killed virus. Two of the others are protein-based vaccines that use a modified cold virus to deliver the protein that will stimulate the immune response.
The final three vaccines in Phase 1 or 2 trials, and the only two in the U.S., are gene-based vaccines. To me, these seem like the most promising.
Gene-based vaccines contain a gene or part of a gene from the virus that causes COVID-19, but not the virus itself. When a person is injected with one of these vaccines, their own cells read the injected gene and make a protein that is a part of the coronavirus. This one protein isn’t dangerous by itself, but it should trigger an immune response that would lead to immunity from the coronavirus.
Gene-based vaccines come in DNA form, like the vaccine in Phase 1 clinical trials from Inovio Pharmaceuticals in the U.S., or in RNA form, like the vaccine in a simultaneous Phase 1/Phase 2 trial from the German company BioNTech and the vaccine in Phase 1 trials from the U.S.-based Moderna.
No gene-based vaccines have ever been approved for human use, but DNA vaccines are used on animals, and a few were in clinical trials for the Zika virus.
In the past, researchers have struggled to develop DNA vaccines that produce strong immune responses, but new techniques look promising. RNA vaccines tend to be more effective in animal studies but have also required innovations before human use. It may be that the time of gene-based vaccines has arrived.
Another benefit of gene-based vaccines is that manufacturers would likely be able to produce large amounts much faster than traditional vaccines. DNA and RNA vaccines would also be more shelf–stable than conventional vaccines since they don’t use ingredients like cell components or chicken eggs. This would make distribution, especially to rural areas, easier.
Still a Long Road to Implementation
The three gene-based vaccines and the five other candidates face many challenges before you or I will be vaccinated. The fact that they are in Phase 1 and 2 trials is encouraging, but the very point of clinical trials is to reveal any problems with a vaccine candidate.
And there are a lot of potential problems. The preclinical results in laboratory animals might not translate well to people. The level of immune protection might be low. And people may react adversely when injected with the vaccine.
Any coronavirus vaccine could also produce a dangerous reaction called immune enhancement, where the vaccine actually worsens the symptoms of a coronavirus infection. This is rare, but has happened with past vaccine candidates for dengue fever and other viruses.
So, how long before we have a vaccine against the COVID-19 virus?
No vaccines have made it through Phase 1 or Phase 2 trials yet, and Phase 3 trials generally take between one and four years. If researchers get lucky and one of these first vaccines is both safe and effective, we are still at least a year away from knowing that. At that point manufacturers would need to start producing and distributing the vaccine at a massive scale.
It is unclear what percent of the population would need to be vaccinated against SARS-CoV-2, but in general, you need to immunize between 80% and 95% of the population to have effective herd immunity. Depending on what the virus does in the coming months, that might not be necessary, but if it is, that’s 260-300 million people in the U.S. alone.
Researchers are doing everything they can to develop a vaccine as fast as possible while still making sure it is effective and safe. Manufacturers can help by preparing flexible systems that could be ready to produce whichever candidate gets across the finish line first.
If everything goes well, Fauci’s 12- to 18-month prediction may be right. If so, it will be thanks to the tireless work of scientists, the support of international organizations and manufacturers all innovating and working together to fight this virus.
About the Author
Marcos E. García-Ojeda, Professor of Molecular and Cell Biology, University of California, Merced. This article is republished from The Conversation under a Creative Commons license. Read the original article.