While a lawsuit alleges that Community Health Systems wrongfully diverted money from its downtown campus to Clovis, one expert says that higher private insurance patient care could be keeping the lights on. (GV Wire Composite/Paul Marshall)

- A lawsuit accused Community Health of wrongfully using money intended for low-income patients and diverting it to the 'wealthier' Clovis hospital.
- An expert painted a dire picture of inadequate Medi-Cal reimbursement rates, saying privately insured patients keep hospital networks afloat.
- Clovis Community Hospital's share of Medi-Cal funding for patients has grown more than any other area hospital.
Share
|
Getting your Trinity Audio player ready...
|
Medi-Cal funding at Clovis Community Hospital falls behind that of other area hospitals, yet it beats the state average of care for low-income patients, a GV Wire investigation found.

“There’s no doubt that those (hospitals) that aren’t disproportionate share are helping subsidize those that are disproportionate share, and isn’t that kind of what’s it all about, setting up arrangements so care can be provided in every area, and not just care, but equitable care?” — Anne McLeod, president/CEO, Private Essential Access Community Hospitals
In addition, 57% of Clovis Community’s revenue comes from government-funded health care — either Medi-Cal or Medicare.
Community Health System’s decision to invest more in Clovis Community than its downtown Fresno hospital in recent years led two local nonprofit groups to sue the network. The social justice advocates claim that the health system wrongfully diverted Medi-Cal money from Community Regional Medical Center, which has one of the highest rates of funding of that kind in the nation.
However, Medi-Cal is a reimbursement for care already provided to a patient, said Anne McLeod, president and CEO of Private Essential Access Community Hospitals. State and federal laws say that Medi-Cal funding can be used where hospital systems deem it most effective.
And, while the suing nonprofits say Community Regional is subsidizing Clovis Community with its better Medi-Cal reimbursement rates — borne from its disproportionate share of low-income patients — McLeod says networks rely on commercial insurance to keep their hospitals financially viable.
“There’s no doubt that those (hospitals) that aren’t disproportionate share are helping subsidize those that are disproportionate share, and isn’t that kind of what’s it all about, setting up arrangements so care can be provided in every area, and not just care, but equitable care?” said McLeod.
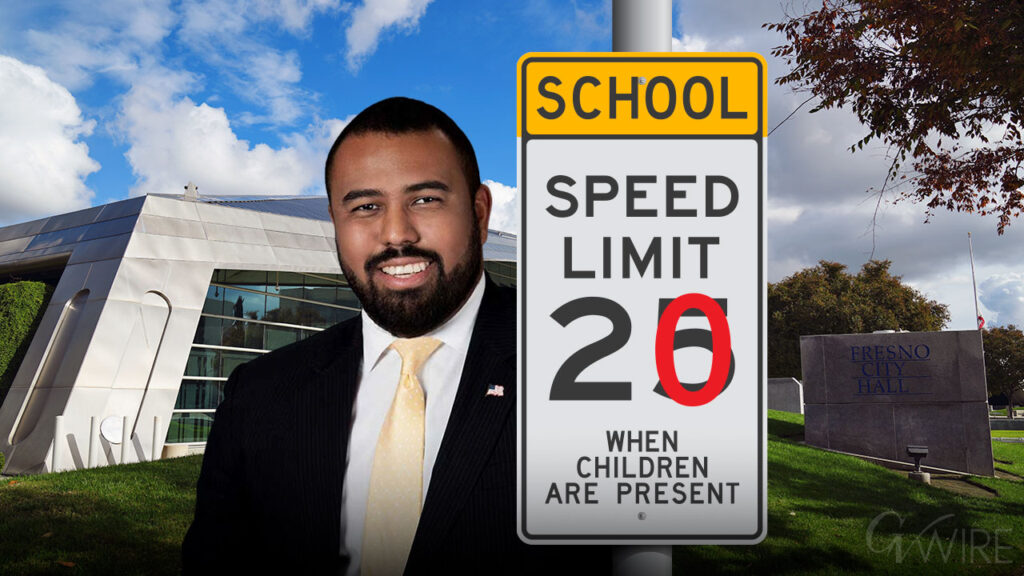
Meanwhile, the Clovis hospital’s share of Medi-Cal revenue has grown faster than any other area hospital over the past five years, according to data filed with the Hospital Care Access and Information.
But, perhaps there is a key fact that everyone can agree on: Medi-Cal reimbursements don’t cover the cost of patient care and are unsustainable for many California hospitals.
Related Story: Lawsuit Alleges Community Health Diverted $1B from the Needy to ...
Safety Net Hospitals Get Additional Medi-Cal Funding
Hospitals get slightly better reimbursement rates when they serve a disproportionate amount of Medi-Cal patients, through what’s called the Disproportionate Share Hospital.
Safety net hospitals that locate themselves in low-income areas get those rates because the state recognizes how insufficient reimbursement rates can be, McLeod said.
Madera Community Hospital closed in part because of its disproportionate share of Medi-Cal patients.
Under another law called the Hospital Fee program — of which McLeod was an author — hospitals pay more to draw on federal matching dollars.
Those programs help offset Medi-Cal funding that doesn’t cover actual cost of care. Even with those better rates, Medi-Cal pays at best 68 cents on the dollar.
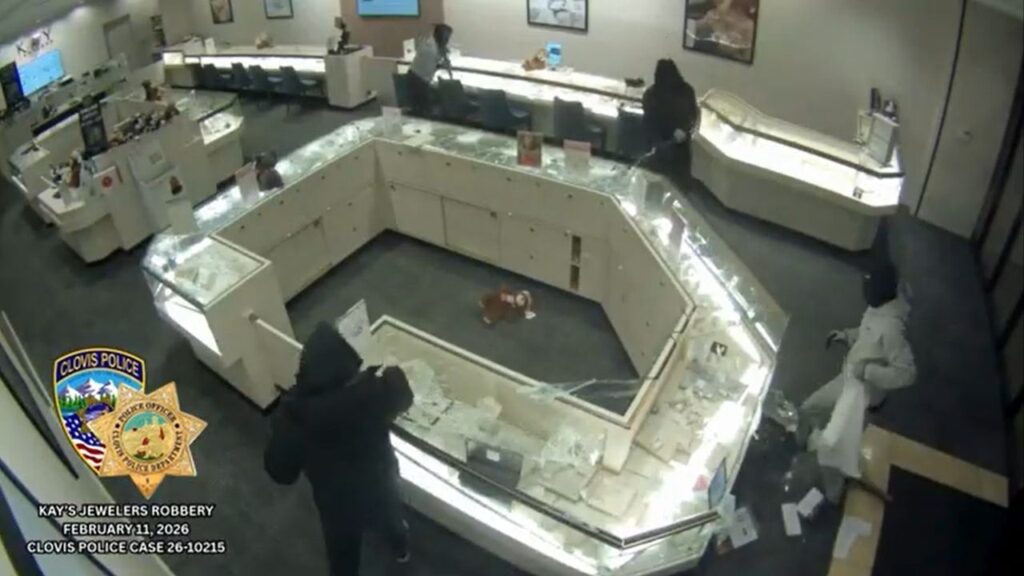
Fresno Building Healthy Communities and Cultiva La Salud sued the nonprofit Community Health System for investing $1 billion to renovate and expand Clovis Community rather than reinvesting those funds in the downtown hospital, which serves a large share of Medi-Cal patients.
“California law required (Community Health) to use Medi-Cal revenue to improve access to quality care for medically underserved populations, especially given that the zip codes most heavily served by Fresno CRMC comprise an area of acute medical need,” the lawsuit states.
McLeod said it’s the better returns from commercial insurance that allow hospital systems to expand care.
Clovis’ Share of Medi-Cal Revenue Grown Fastest in 5 Years
The percentage of Medicaid patients — called Medi-Cal in California — at Community Regional is among the highest in the nation, McLeod said. In 2023, 49% of outpatient discharges were from Medi-Cal patients, according to data from HCAI. And, nearly 52% of inpatient days were from Medi-Cal patients.
Medi-Cal funding made up 39.15% of patient revenue in 2023, compared to a 21.7% average statewide. Becker’s Hospital Review calculated the statewide average using the most recent data available.
Clovis’ payer mix had 21.99% Medi-Cal. The $4.3 million in indigent care provided at Clovis Community in 2023 also outpaced any other area hospital, including St. Agnes, which had the second highest rate.
Clovis’ share of Medi-Cal revenue has also risen more than any other hospital in the past five years. Medi-Cal funding made up 14.56% in 2019.
Community Regional and Adventist Health Hanford grew about 2 percentage points in that time period, while Kaweah Delta Medical Center grew nearly 4 percentage points.
St. Agnes’ Medi-Cal share declined nearly 6 percentage points.
California Hasn’t Increased Medi-Cal Reimbursement Rates
McLeod said California’s Medi-Cal reimbursement is unsustainable, requiring hospitals to rely on private or commercial insurance to offset losses from Medi-Cal patients. That means more money to advance care.
“Medi-Cal only pays, with all the funding included…about 68% of the actual cost required to provide care to those patients,” McLeod said.
The share of Medicaid paid to states varies. Some southern states need only put up 20% of cost to receive 80% from the feds. California has to pay 50%. But California made it clear in 2009 that it didn’t want to fund that full amount, leaving it to hospitals to contribute to a fund to draw the full amount of federal money. That program is called the Hospital Fee program.
“California has either been unable or unwilling to make that kind of investment in the Medi-Cal program. It is abysmal and it is irresponsible to have a program of 14 million people on it and you don’t even come close to covering the cost of care,” McLeod said.
And with the Affordable Care Act and other California legislation, approximately one-in-three people are on Medi-Cal, McLeod said. Combined with Medicare, some safety net hospitals have 86% of patients being government funded.
More than 76% of Community Regional’s funding comes from either Medicare or Medi-Cal. The combined is 57% at Clovis Community, which the lawsuit characterized as serving “a much wealthier, whiter, and healthier population.”
Even as the number of people on Medi-Cal has grown and the cost of doing business has climbed, the funding percentage that the state of California pays into the program has not increased.
“Health care costs grow, pharmaceuticals increased, labor increases the cost of doing business and interest,” McLeod said.
Thus, hospitals have been forced to pay more to access matching federal dollars. In 2009, hospitals paid around $1 billion; that figure is closer to $5 billion now, McLeod said.
Of the money the federal government gives to the hospital fee program, California taxes 24%, which goes into the state’s general fund, McLeod said.
“Technically in the law, it’s used to pay for children’s health care coverage, but it just goes to the general fund,” McLeod said.
No Restriction on How a Hospital Spends Medi-Cal Money
McLeod said there is no requirement on how a hospital network spends Medi-Cal reimbursements, whether it goes to Clovis Community or Community Regional.
The nonprofits’ lawsuit against Community Health System seeks to have a court rule that Medi-Cal reimbursements must remain at the hospital where the patient received care.
McLeod said that the Medi-Cal funds are a reimbursement for services the hospital provided and the money arrives sometimes up to two years after a patient is treated.
“They’re using that money to fulfill that obligation that kept them open and whole when they were incurring losses on caring for those patients,” McLeod said. “It’s like you just got your paycheck two years in arrears and you were living off your credit card. You’re going to now pay your credit card off, right?”