Share
California’s community colleges don’t offer a pipeline facilitating a student’s ability to attend medical school. But Senate Bill 40 by state Sen. Melissa Hurtado, D-Sanger, seeks to fix that, and it has unanimously passed the Senate Health Committee.
“We’re in a provider shortage in the Valley that’s already bad,” says Hurtado. “We need to make sure that we create a way that streamlines the educational system so all students across the state can have an opportunity to become doctors.”

“We need to make sure that we create a way that streamlines the educational system so all students across the state can have an opportunity to become doctors.” –State Sen. Melissa Hurtado, D-Sanger
SB 40 would create the California Medicine Scholars Program, a 5-year pilot program commencing Jan. 1, 2023, and requiring the Office of Statewide Health Planning and Development to establish and facilitate the pilot program.
“It would create a pathway from community college and or CSU to get into medical school,” said Hurtado.
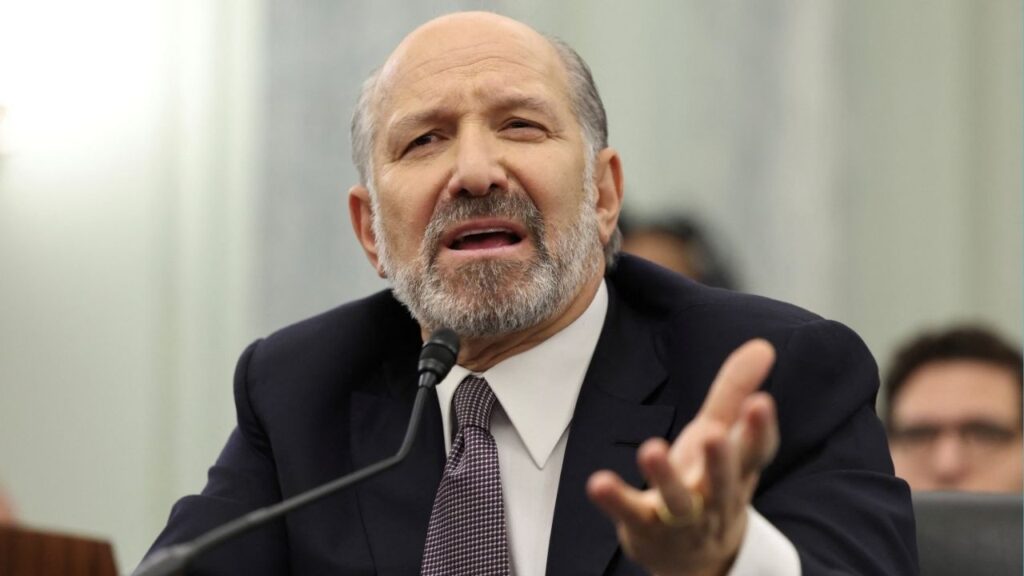
One of the bill’s co-authors, Sen. Anna Caballero, D-Salinas, believes it’s a great bill that will make investments where they’re most needed.
“To be able to train young people from the Central Valley who will then stay here and work for families in the Central Valley,” said Caballero. “We’ve been trying to get a medical school here as well. Creating the pathway is really important.”
Regional Hubs of Health Care Opportunity
The pilot program would consist of four Regional Hubs of Health Care Opportunity. At least one of the hubs would be in the Central Valley.
Among the hubs’ features are:
- Scholarships
- Internships
- Shadows of clinical rotations
- Research or community service to ensure students gain a familiarity with the needs and challenges for primary care in their region.
4,000+ Doctors Short By 2030

“We’ve been trying to get a medical school here as well. Creating the pathway is really important.”– State Sen. Anna Caballero, D-Salinas
According to a 2017 report from the University of California San Francisco Healthforce Center, California is predicted to see a shortage of over 4,000 primary care clinicians by 2030.
In the Central Valley, Inland Empire, and Imperial Valley, communities are already experiencing the pains of a shortage. Patients in these regions face longer than average wait times to see a physician or extensive time to travel to the closest physician, according to language in the bill.
Central Valley Medical Schools
Although the need is great in the Inland Empire, that region, unlike the San Joaquin Valley, has an established government-funded medical school at the University of California, Riverside.
A second, privately funded medical school, the California University of Science and Medicine in San Bernardino County, was accredited in 2018.
In the Central Valley, there are nascent efforts to establish a government-funded medical school presence through UCSF Fresno and the San Joaquin Valley Program in Medical Education program. Also developing is UC Merced’s Medical Education Collaborative.
On the private front, there is California Health Sciences University in Clovis. The CHSU College of Osteopathic Medicine building opened in early 2020. The new medical school has three large classrooms, an Osteopathic Skills lab, library, plentiful private and collaborative study spaces, and a simulation center.
(Disclosure: GV Wire Publisher Darius Assemi serves on CHSU’s Board of Trustees.)
Hurtado wants her bill to pivot the Central Valley from a medical desert to an oasis for prospective students.
“It would benefit students that come from disadvantaged communities,” explains Hurtado.

Underrepresented Populations
Researchers from UCLA’s Latino Policy & Politics Initiative (LPPI) reported in 2018 that the scarcity of Latino physicians in California has led to a deficit of 54,655 Latino physicians required to achieve parity with non-Latino white physicians.
Should existing trends in recruitment and training of physicians in the state efforts continue, LPPI researchers calculated it will take California five centuries to achieve parity.
Researchers have also found that African American and Latino doctors are more likely to practice in communities that reflect their cultural background. Further studies have found evidence that the gaps in mortality between African American and white patients can be reduced when African American patients are treated by African American physicians.
[activecampaign form=25]